Leading Oncofertility Care
Take a moment and imagine this: A doctor has just told you your child has cancer.
The good news is most children survive. You’re told chemotherapy will start next week. You’re given information booklet after booklet. Told about clinical trials. Consented to clinical trials. Referred to social work, to a nutritionist, for more appointments, scans and tests.
You are overwhelmed, scared and exhausted.
Then a doctor tells you that the lifesaving treatment your child is about to have, may cause infertility. That is, it might not be possible for them to have children later in life.

Fertility preservation is any medical procedure undertaken with the intent of preserving the ability to conceive a child, and carry the pregnancy through to a live birth. Some technologies have established efficacy, others remain experimental. With all procedures though, there is no guarantee of a live birth.
Now you’re asking yourself: Do I want my child to have another procedure? What are the risks? What are the benefits? How do I make the best decision?
Research tells us that parents feel overwhelmed and under informed. It also tells us that there is no right or wrong decision. It is the discussion about fertility and information provision that is important. With information, parents feel empowered to participate in shared-decision making, are more satisfied with their decisions, and are less likely to experience decision regret.
Research indicates healthcare providers can struggle to discuss the impacts of cancer treatments on fertility. There are vast differences in health service funding, research and health centre capabilities to offer fertility care. Despite the many challenges, however, oncofertility (the study of cancer and cancer treatment impacts on fertility) continues to rapidly advance.
In 2012, in response to calls from cancer survivors and their families, a multidisciplinary taskforce involving major Victorian Comprehensive Cancer Centre (VCCC) partners was established across the paediatric and adult sectors to address the unmet needs around fertility. Respectful exchange has enabled the introduction of new ethical and integrated models of care.
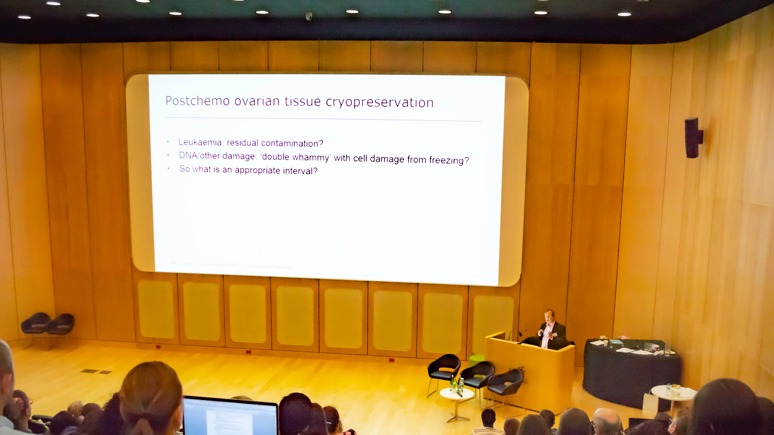
In December 2019, the Fertility Preservation Taskforce hosted the second National Oncofertility Summit at The Royal Children’s Hospital. Partners contributing to this event included The University of Melbourne, The Royal Women’s Hospital, The Youth Cancer Action Board Peter MacCallum Cancer Centre and Fertility Preservation Taskforce Consumer Advisory group. This summit was supported by a Melbourne Medical School (MMS) strategic grant.
The Summit attracted 180 national and international delegates. There were 65 scholarships awarded to support allied health, nurses, student, consumers and ANZCHOG nominees to attend and enable capacity building in the sector. Highlights included five international speakers, a consumer-led session and a global champions pecha-kucha.
The head of the FP Taskforce, Dr Yasmin Jayasinghe, Winter and Glover Cancer Research Fellow, Department of Obstetrics and Gynaecology, was interviewed by Channel 9 News.